
Here to serve the people of Montana and its livestock industry.
Animal Health Bureau
- Permits & Forms
- Brucellosis
- Brucella canis
- Feral Swine
- High Path Avian Influenza
- Johne's
- Rabies
- Trichomoniasis
- West Nile Virus
- National Poultry Improvement Program (NPIP)
- Pay for Permits Online
Helpful Links
Contact Information
Department of Livestock
Animal Health Bureau
PO Box 202001
Helena, MT 59620-2001
Email: livpermits@mt.gov
Rabies
- Montana Regulations
- Current Quarantines
- Rabies in Montana
- Disease Information
- Prevention
- What is the risk for my pet?
- Signs & Symptoms
- What do I do if I suspect an animal of having rabies?
- Diagnosis
- Treatment
- Additional Information
Domestic animals with suspected rabies exposure may be subject to action based upon Administrative Rules of Montana (ARM). Potential actions include booster of rabies vaccination, 45 day observation, 120 day quarantine, and euthanasia. The Rabies Exposure Assessment Tree can be used as a guide for suspected rabies exposure in dogs, cats and ferrets. Please note, all suspected exposures must be reported to MDOL immediately.
Counties are placed under a 60-day quarantine when rabies is confirmed in a terrestrial animal such as a dog, cat, skunk, etc. All unvaccinated dogs, cats and ferrets in quarantined counties must be vaccinated a minimum of twenty-eight (28) days prior to any travel outside the county. Quarantine release dates are subject to change.
Current County Rabies Quarantines
| County | Species | Effective Date | Release Date |
| There are no rabies quarantines at this time |
2025 Positive Rabies Cases
| Month | County | Species |
| September | Flathead | Bat |
| September | Gallatin | Bat |
| September | Silver Bow | Bat |
| September | Ravalli | Bat |
| September | Galatin | Bat |
| September | Flathead | Bat |
| September | Flathead | Bat |
| September | Ravalli | Bat |
| September | Lincoln | Bat |
| August | Missoula | Bat |
| August | Flathead | Bat |
| August | Flathead | Bat |
| August | Sanders | Bat |
| August | Lincoln | Bat |
| August | Flathead | Bat |
| August | Missoula | Bat |
| August | Gallatin | Bat |
| July | Lewis & Clark | Bat |
| July | Missoula | Bat |
| July | Rosebud | Bat |
| July | Yellowstone | Bat |
| July | Lewis & Clark | Bat |
| July | Flathead | Bat |
The map below represents Montana rabies cases for FY25 (7/1/2024-6/30/2025) by county. Click the map to display the interactive map with more in-depth detail.

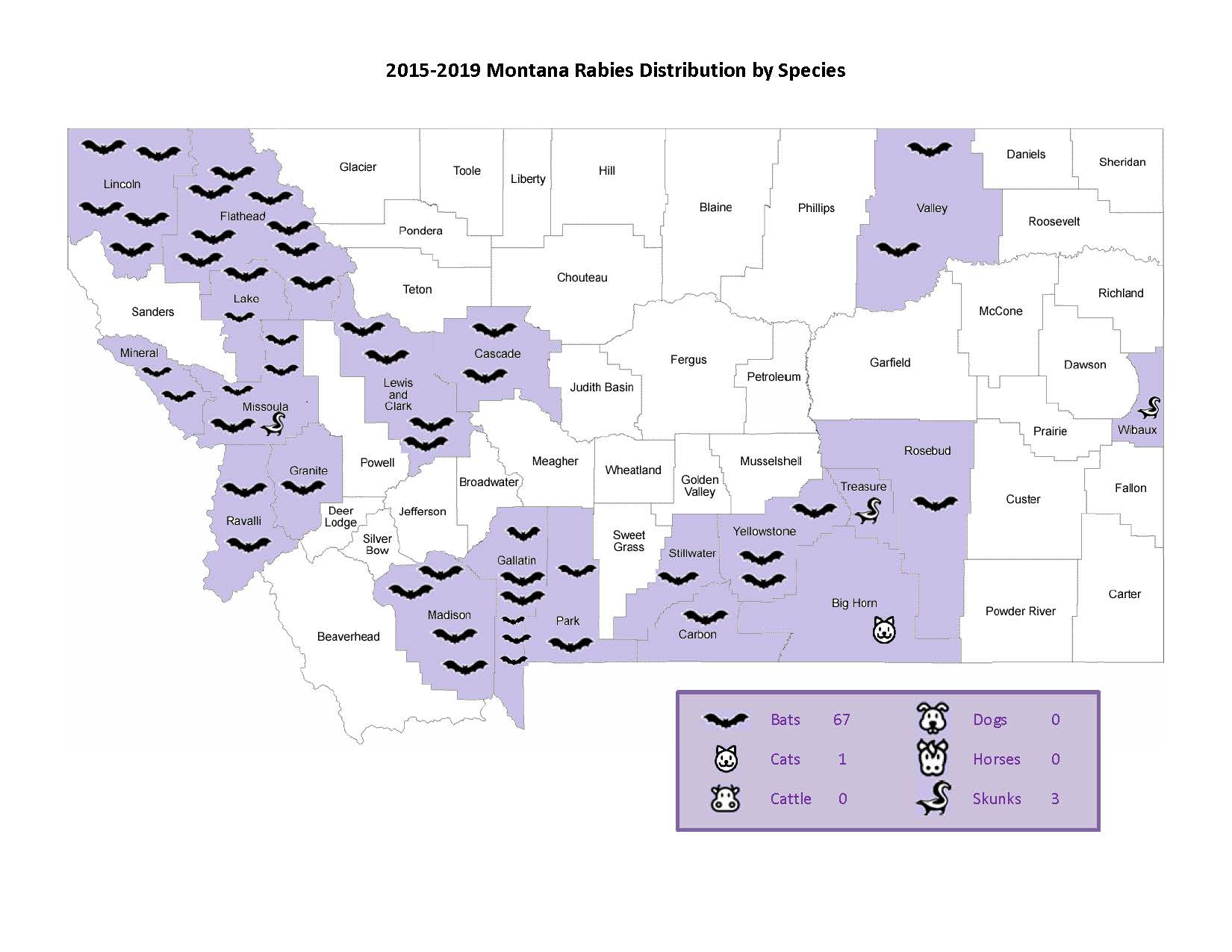
2015-2019 Montana Rabies Distribution by Species
(view PDF)
Historical Rabies Distribution Information:
- 2009
- 2010
- 2011
- 2012
- 2013
- 2014
- 2015
- 2016
- 2017
- Fiscal Year 2020 (July 1, 2019 - June 30, 2020)
- Fiscal Year 2021 (July 1, 2020 - June 30, 2021)
- Fiscal Year 2022 (July 1, 2021 - June 30, 2022)
- Fiscal Year 2023 (July 1, 2022 - June 30, 2023)
- Fiscal Year 2024 (July 1, 2023 - June 30, 2024)
Rabies is a deadly but preventable viral disease that affects all species of mammals, including humans. The virus infects the central nervous system, causing swelling of the brain (encephalitis) and ultimately death. There is no cure for animals that contract the disease, which is always fatal to the infected animal.
Rabies is generally transmitted by the saliva of infected animals, most commonly through bites or scratches. Infection can also occur when infective saliva comes into contact with open wounds such as cuts and scratches or mucous membranes (eyes, nose or mouth).
Most rabies cases in the U.S. involve wild animals, mostly skunks, bats, raccoons, coyotes and foxes. In Montana, skunks and bats account for more than 90 percent of all reported cases. Distribution in Montana is statewide.
Rabies in humans is almost always fatal unless treated before symptoms appear, but is a rare event in the U.S. with 1-2 deaths per year. Globally, the disease accounts for more than 55,000 human deaths a year, mostly in Asia and Africa.
Back to top
Prevention
There is no treatment for rabies in infected animals; thus, prevention is the first line of defense. Currently, effective and inexpensive vaccines are available for dogs, cats, sheep, cattle, horses and ferrets. MDOL recommends that all dogs, cats and ferrets be vaccinated for rabies, however there is no statewide vaccination requirement in Montana. Rabies vaccination requirements are regulated by individual cities and counties. Please consult your veterinarian for local regulations. Other "best management practices" can also be used to reduce the risk of exposure to rabies:
- Always vaccinate your pet(s)! Work with your veterinarian to develop a pet health plan that includes rabies and other important vaccinations;
- Make sure your pet's booster vaccinations are up to date;
- Enjoy wildlife from a distance;
- Keep your pets from running at large to reduce exposure to wild animals;
- Avoid any animals acting unusual (see Symptoms);
- Report a description and location of suspect animals to local animal control officers or the county sheriff's office as quickly as possible;
- Conduct a thorough inspection of your residence and property: Eliminate attractants that draw wildlife (pet food, garbage cans without lids, etc.); block entry points wild animals might use to access foundations, porches, steps and roofs; eliminate sites that might be used for sleeping or nesting; use night or motion lights to discourage nocturnal animals; etc. Managing wild animals that most commonly carry the disease can reduce your risk of exposure.
In regard to livestock, the decision to vaccinate rests solely with the owner. Given the risk – rabies in livestock is rare in livestock – it is generally not practical to vaccinate livestock on a large basis.
Human vaccines are also available, and are recommended as a preventive measure for high-risk individuals such as veterinarians, animal handlers and laboratory workers.
Anyone who is bitten or scratched by an animal of unknown rabies and/or vaccination status should immediately and thoroughly wash the wound with soap and water and seek medical attention for the wound. Animal bites should be reported to the county health department (or county sheriff's office after hours) as soon as possible.
Back to top
What is the risk for my pet?
Any animal bitten or scratched by a wild, carnivorous mammal, bat or pet that cannot be tested or is of unknown vaccination status should be considered as having been exposed to rabies.
Unvaccinated dogs, cats, and ferrets exposed to a rabid animal should be euthanized immediately . If the owner is unwilling to euthanize, the animal must be quarantined in strict isolation for six months. Animals with expired vaccinations need to be evaluated on a case-by-case basis. Exposed dogs and cats that are current on vaccinations must be kept under observation in less stringent confinement for 45 days.
Small mammals such as squirrels, rats, mice, hamsters, guinea pigs, gerbils, chipmunks, rabbits and hares are seldom found to be infected with rabies and have not been known to cause rabies among humans in the U.S. Bites by these animals are usually not considered a rabies risk.
Pet owners can learn more about rabies in their area by checking the department's web site for current quarantines, press releases and other information. Additionally, while vaccination is NOT required statewide for dogs, cats and ferrets, vaccination requirements may vary from place to place; local veterinarians are good sources of information about local vaccination requirements and rabies in your area.
Back to top
Signs and Symptoms
Abnormal behavior is the most consistent sign of the disease in animals.
Rabies can take on two forms in animals – dumb or furious. With the dumb form, animals become shy or hide, and are often unapproachable. They may be sluggish and act depressed or confused. With the furious form, animals are excitable, irritable and aggressive, and may suddenly attack if approached. Other signs of rabies include drooling; inability to eat, drink or swallow; frothing at the mouth; and staggering, weakness, convulsions and paralysis. Animals will normally become comatose prior to death.
In people, rabies first manifests with general, nonspecific flu-like symptoms - malaise, fever or headache. As the disease progresses, patients may experience mental dysfunction, anxiety, confusion, agitation, delirium, abnormal behavior, hallucinations, convulsions, insomnia and paralysis. Death generally occurs one to two weeks after the onset of symptoms, although the incubation period can run as long as 90 days.
Back to top
What do I do if I suspect an animal of having rabies?
If you encounter an animal you suspect of having rabies, the first rule is always protect yourself and your pet against exposure. A description of the animal and location should be reported to local animal control officers or the county sheriff's office as soon as possible.
Generally, you should never handle or attempt to handle an animal suspected of having rabies. However, due to Montana's rural nature and the unavailability of animal control officers in some parts of the state, it may be necessary to collect a sample yourself. If you are collecting a specimen to submit for testing, always wear heavy, puncture-resistant gloves when handling the sample, and double-bag all samples. Care should be taken to leave the head of the suspect animal as intact as possible to preserve the suitability of the sample for testing.
Back to top
Diagnosis
The direct fluorescent antibody test (dFA) is the test most frequently used to diagnose rabies in animals. This test requires brain tissue from animals suspected of being rabid, and can only be performed post-mortem.
Several tests are necessary to diagnose rabies ante-mortem (before death) in humans; no single test is sufficient. Tests are performed on samples of saliva, serum, spinal fluid and skin biopsies of hair follicles at the nape of the neck. Saliva can be tested by virus isolation or reverse transcription followed by polymerase chain reaction (RT-PCR). Serum and spinal fluid are tested for antibodies to rabies virus. Skin biopsy specimens are examined for rabies antigen in the cutaneous nerves at the base of hair follicles.
Back to top
Treatment
There is no cure for rabies in animals, and the disease is always fatal.
In humans, rabies is almost always fatal once signs of the disease develop. People bitten or scratched by ANY ANIMAL of unknown rabies or vaccination status should immediately wash the wound with soap and water and seek medical assistance.
Treatment for people, known as post-exposure prophylaxis, consists of a combination of rabies antiserum and a series of vaccinations.
Back to top
- 2016 Compendium of Animal Rabies Prevention and Control
- Rabies ARM
- Rabies Exposure Assessment Tree
- Montana Department of Public Health & Human Services
- Centers for Disease Control
- USDA-APHIS Wildlife Services
- American Veterinary Medical Association
- MCA 50.23 Part 1: Restrictions on Possession of Wild Animals
